If you’re a drug/alcohol treatment clinician, or a physician, or a counselor, or if you’re an alcoholic, or a drug user, or a smoker, I’m sure you’ve advocated for and tried every approach to quitting, detox, recovery and relapse prevention you can think of – but I’m also pretty sure you haven’t tried the one I’m going to describe here. It’s so simple and obvious that I hope it will make you say “Duh” and then give it a try.
In the world of addiction treatment and recovery, clinicians try to identify and monitor every variable that might affect a patient’s ability to detox, heal, and stay sober and/or drug-free.
Yet there is one high impact – and 100% preventable – relapse factor that almost universally escapes clinical attention because it’s fully accepted as something totally ordinary, and it’s always in plain sight.
It’s the cigarettes. While every treatment professional is probably aware of the well-documented association between smoking and drug/alcohol relapse, I’m pretty sure that few are aware that it’s not the tobacco, and not the Nicotine that creates the strong link between smoking and relapse. I’ll explain.
The cigarettes that 60-70% of people in detox and rehab smoke are heavily contaminated with undocumented, unregulated neurotoxic, dopaminergic, endocrine-disrupting pesticides that themselves have multiple highly addictive properties. I want to show you how it’s very likely not the smoking itself causing detox/relapse failure, it’s the pesticides in the smoke. I’ll show you why that happens and how it can be easily managed in a way that doesn’t involve quitting.
First, on the relationship between a higher risk of relapse and smoking:
Cigarette smoking and risk of alcohol use relapse among adults in recovery from alcohol use disorders
https://pmc.ncbi.nlm.nih.gov/articles/PMC4592419/#
“Alcohol consumption and cigarette use are frequently co-occurring behaviors that can have negative impacts on the health of adults. The current data suggests that both daily and non-daily cigarette smoking are associated with a greater risk of relapse to AUDs among adults in the U.S., which is consistent with data from clinical treatment settings.”
Smoking relapse risk is increased among individuals in recovery
https://pmc.ncbi.nlm.nih.gov/articles/PMC6685745/
“Cigarette smoking and drug and alcohol use share similar environmental, social, and behavioral factors, in addition to similar biochemical endogenous reinforcement suggesting common underlying mechanisms (Biederman et al., 2006).
“For instance, nicotine and other substances produce similar reinforcing dopaminergic effects in the ventral tegmental area of the mid-brain and the nucleus accumbens (Nestler, 2005) and chronic exposure to nicotine and other substances can impair dopaminergic responses to reward and cause long-term sensitization of the dopaminergic system after discontinuation of use (Koob, 2009; Koob and Le Moal, 2008a, b).
“Thus, the neuroplasticity that supports the development and maintenance of SUDs might influence the ability to discontinue tobacco use and vice versa. Specifically, several recent studies suggest that cigarette use is associated with increased risk of SUD relapse (Weinberger et al., 2017), and alcohol and cannabis use are associated with increased risk of persistence of cigarette use and relapse among former smokers (Weinberger et al., 2018).”
It’s also well-established that smokers in detox and rehab don’t want to quit, to put it mildly, and clinicians don’t fight it because they’ve been trained to think of of cigarette smoking as nicotine addiction, a relatively minor issue compared to alcohol and drugs. Also a significant number of rehab staff are also smokers themselves, further reducing their level of concern.
The problem is that the pesticide residues that contaminate every commercial cigarette brand are relapse-driving neurotoxic, hepatotoxic, diabetogenic, and endocrine disrupting substances, interacting invisibly but powerfully with the already fragile physiology of someone in toxic withdrawal from drugs or alcohol to drive them back into using in spite of every effort to stay clean.
That’s because smokers are dealing with an unrecognized toxic synergy – far more than tobacco and nicotine – that invisibly intensifies their alcohol/drug detox & withdrawal symptoms, delays, interferes with, and prevents healing, and greatly increases their risk of relapse.
The idea that inhaled pesticides could be adding unrecognized addictive properties to cigarettes may seem novel, but since the topic of pesticides in cigarettes has been totally absent from medical or scientific discussion for 75 years it’s not surprising.
What may be surprising is what we can see when we simply ask the question: “Are the multiple synergistic pesticide contaminants in cigarettes reinforcing the addictive properties of drugs and alcohol”?
Pesticide Found In Cigarettes That Reinforce Drug/Alcohol Addiction
| Pesticide | Dopaminergic Reward Activation | Neuroadaptation | Stress & Withdrawal Circuits | Neuroplastic Changes |
| Acetamiprid | Possible indirect activation via nAChRs | Cognitive impairment; fetal brain accumulation | May affect amygdala via neurotoxicity | Alters brain development in animal studies |
| Bifenthrin | Indirect dopamine impact via sodium channel disruption | Behavioral changes in rodent studies | Anxiety-like behavior observed | Synaptic function alterations, developmental effects |
| Cypermethrin | May elevate dopamine via sodium channel modulation | Behavioral sensitization in animals | Induces anxiety/stress-like responses | Structural changes in hippocampus and cortex |
| DDT | Endocrine disruption may affect dopamine | Long-term exposure alters behavior | Stress hormone dysregulation | Neurodevelopmental changes linked to exposure |
| Ethofenprox | Potential dopamine modulationpyrethroid- like | Behavioral adaptation in animal models | May trigger stress responses | Chronic exposure alters synaptic function |
| Imidacloprid | Activates nAChRs affecting dopamine | Evidence of neural toxicity in developmental models | May influence stress circuits | Alters neural architecture in fetal exposure models |
| Indoxacarb | Limited evidence for dopaminergic activity | Unknown adaptation effects | Unclear withdrawal response | No confirmed neuroplastic changes |
| Permethrin | Disrupts neuronal sodium flow; indirect dopamine impact | Behavioral changes observed | Anxiety-like responses linked to exposure | Affects neurodevelopment and synaptic signaling |
| Tetramethrin | Similar to other pyrethroids; possible dopamine link | Suggestive signs of adaptation in repeated use | Unknown stress pathway activation | Limited data on structural neural change |
| Thiacloprid | Modulates nAChRs, potentially influencing reward pathways | Developmental neurotoxicity noted | Potential links to stress response | Changes in brain structure in early exposure |
| Spinosad | Alters nAChRs and GABAergic transmission; reward impact unclear | Tolerance effects unknown | No direct withdrawal data | Limited neuroplastic research available |
Alcohol Withdrawal Meets Pesticides
Alcohol/Drug withdrawal is a physiological and psychological storm where the brain and central nervous system, deprived of alcohol’s depressant effects, become hyperexcitable. GABAergic tone drops, glutamatergic activity spikes, and the brain enters a volatile state. Symptoms like seizures, anxiety, delusions, panic attack, insomnia, and delirium tremens are common.
Now layer in chronic daily exposure, +/- 200 inhalations per pack, to multiple pesticides like cypermethrin, bifenthrin, DDT, and imidacloprid – compounds that are known to disrupt neurotransmitter systems including GABA, dopamine, and acetylcholine, the same systems that are under stress from withdrawal.
These chemicals don’t just add stress; they create their own and then amplify the whole package. They invisibly worsen the imbalances that withdrawal creates, pushing the brain and CNS further into instability.
Breathing and Blood Pressure
Withdrawal and detox doesn’t just affect the brain and CNS – it taxes the heart and lungs. Elevated heart rate, blood pressure spikes, and respiratory discomfort are routine.
But pesticides like permethrin, tetramethrin, and ethofenprox, inhaled as a cocktail through cigarette smoke 100-200 time a day, are known to attack and compromise these systems as well.
The result? Worsened tachycardia, hypertension, and breathing difficulties. For patients already in a fragile state, this added burden can also tip the scales toward medical complications and relapse.
The Liver & Toxicity
The liver plays a central role in alcohol detox, processing ethanol and metabolizing medications like benzodiazepines. But it’s also responsible for breaking down pesticides, many of which are hepatotoxic and processed by the same CYP450 enzymes.
Compounds like alachlor, carbendazim, metalaxyl, and thiophanate-methyl don’t just add to the liver’s workload; even with individual exposure they compete with alcohol and detox medications for metabolic resources, but when inhaled in multiples the synergy is toxic overload.
This dual burden can delay alcohol clearance, increase inflammation, and interfere with treatment protocols.
Mood, Cravings, and Cognitive Fog
Recovery isn’t just physical – it’s emotional and psychological. Patients in detox often struggle with depression, anxiety, and cravings. Pesticides such as imidacloprid, fluopyram, and azoxystrobin disrupt dopamine and serotonin pathways, deepening emotional instability, a condition that’s then reinforced by hundreds of exposures a day in heavy smokers.
These effects aren’t abstract. They manifest as heightened irritability, intensified cravings, and impaired decision-making – all of which increase the risk of relapse, especially when smoking is being used and even approved as a coping mechanism (such heavy irony!).
Endocrine Disruption
Alcohol withdrawal affects cortisol and sex hormones, destabilizing sleep, appetite, and stress response.
Pesticides like DDT, pendimethalin, and tebuconazole are well-known endocrine disruptors that compound this chaos, but they have never once been identified by any agency as tobacco product contaminants. Crickets from FDA about pesticides in cigarettes.
The result is a hormonal storm: disrupted circadian rhythms, increased stress reactivity, and metabolic shifts that make recovery harder and cravings stronger.
Synergistic Toxicity
Some non-pesticide additives, such as piperonyl butoxide and MGK-264, are designed to inhibit enzymes and boost pesticide potency. In the context of alcohol withdrawal, this is a recipe for amplified toxicity and slower clearance.
These synergists don’t just make pesticides more potent – they make them linger longer, increasing the risk of unexpected reactions and compounding the body’s toxic load.
The Big Picture: Chronic Pesticide Exposure and Detox Disruption
When we zoom out, the implications become even more alarming. Chronic low-level exposure to multiple pesticides through smoking, involving hundreds of contaminated smoke inhalations a day for even pack-a-day smokers, creates a cascade of complications:
- Neurological Disruption: Pesticides interfere with neurotransmitter function and gut-brain signaling, worsening mood instability and cognitive fog.
- Liver Overload: Dual hepatotoxicity from alcohol and pesticides overwhelms detox pathways and depletes glutathione, a key antioxidant.
- Endocrine Chaos: Hormonal imbalances increase cravings and complicate withdrawal.
- Gut Damage: Disrupted microbiome and leaky gut syndrome trigger systemic inflammation and fatigue.
- Bioaccumulation: Lipophilic pesticides stored in fat tissue may be released during detox, intensifying symptoms.
Recovery at Risk: Why This Matters
The consequences of pesticide exposure during alcohol detox are not theoretical – they’re clinical and they’re serious. Because of this unrecognized exposure, patients face:
- Slower healing and prolonged withdrawal
- Increased risk of liver disease, including cirrhosis and fibrosis
- Greater vulnerability to relapse due to mood instability and cravings
- A need for enhanced nutritional and antioxidant support to offset toxic burden
However, if encouraged, educated, and even incentivized to transition to cigarettes free from pesticide contamination, patients will experience:
- Shortened withdrawal duration
- Reduced toxic burden on the liver and brain
- Improved emotional stability and reduce cravings
- Enhanced responsiveness to treatment protocols
- Measurable improvements in recovery outcomes
- Reduced short & long-term relapsing
- Enhanced ability to taper and quit smoking
A Simple, Actionable Solution
Given the evidence, addiction treatment centers have a clear opportunity to improve outcomes: educate, encourage and even incentivize patients to switch to pesticide-free cigarettes.
This intervention doesn’t require major infrastructure changes or costly programs. It simply acknowledges a hidden threat and offers a safer alternative. By eliminating chronic multi-pesticide inhalation exposure, clinics can ease alcohol and drug withdrawal symptoms, support metabolism and liver function, and help patients stay on the path to recovery.
Pesticide-free cigarettes may seem like a minor detail in the detox process – but when they’re laced with neurotoxins and endocrine disruptors, they become a major and 100% avoidable obstacle. It’s time to bring this issue into the light and give patients every possible advantage in their fight for sobriety.
For decades the tobacco industry and the US Government have squashed any research into the impact of pesticides in cigarettes smoke, so it’s going to be up to individual programs to quietly give this approach a try. I suggest not seeking public funding or making any kind of announcement but quietly working with a small group of smokers in your rehab program, educating them on what’s going on, and helping them switch to pesticide-free organic tobacco cigarettes – then seeing what happens. You and they may just be amazed. If you have to buy them the organic tobacco cigarettes for the first month to get their willing participation then even a pack-a-day smoker will cost only about $250 – how does that compare with the cost of treatment that isn’t working all that well anyway?
One final point. Every Alcohol/Drug treatment program would prefer that their patients stop smoking, but understand that alcohol and drug abuse take precedence. However, there’s plenty of anecdotal evidence that SUD or not, smokers who switch to pesticide-free tobacco cigarettes automatically smoke fewer cigarettes, and find it much easier to taper and quit if they choose to do so.
Do you see any downside to giving this approach a try?
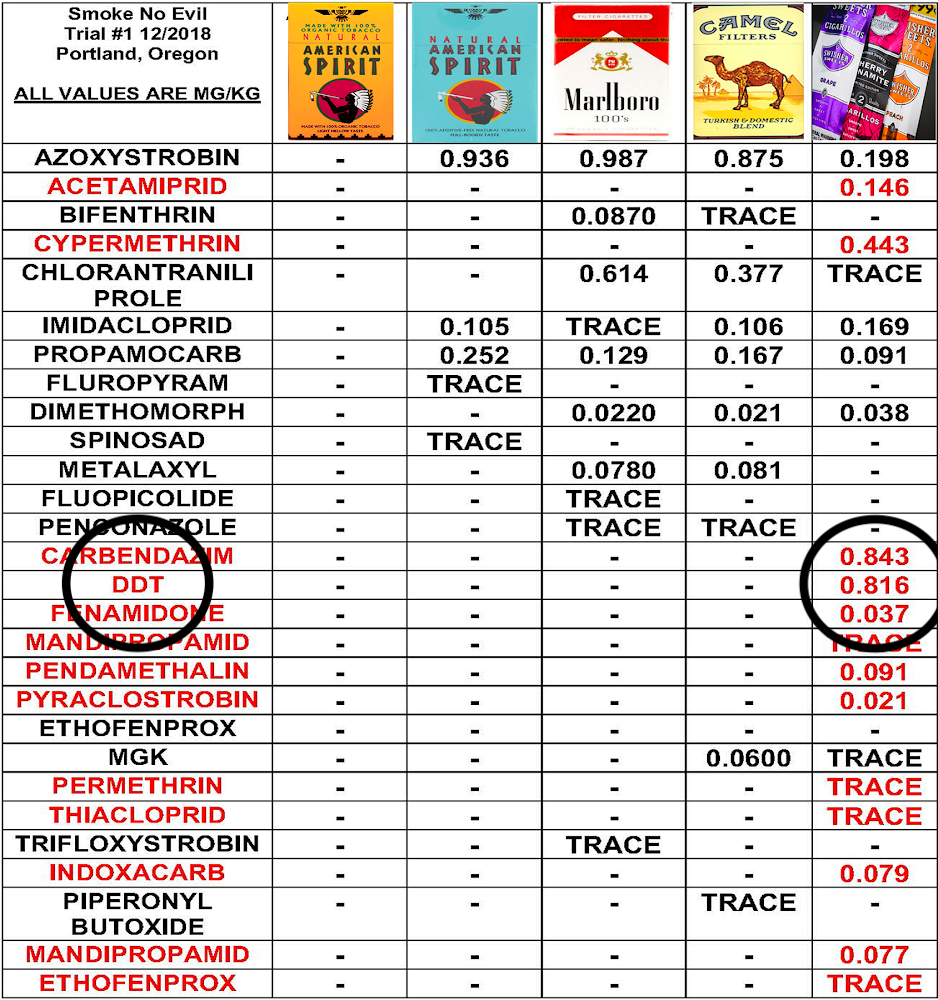
Just in case the idea of pesticide contaminants in cigarettes doesn’t compute – here’s the evidence. And notice the American Spirit organic brand on the left in this first graphic. Zero pesticides, available everywhere. There’s your new approach to relapse prevention – readily available, already accepted by 1 million+ US smokers, and free from pesticides. Plus a strong history of reduced urges to smoke, fewer cravings, and ease of tapering down even to zero.